NHS consultants’ vote for strike action: Enter the Knights and Knaves
NHS Consultants have voted to take strike action, which if it happens, will be an historic event in the NHS. More than 24,000 consultants voted in the British Medical Association’s ballot, representing a 71 per cent turnout, with 86 per cent saying they were prepared to strike. Walk-outs are planned for the 20th and 21st July. A ‘Christmas Day’ type of emergency cover will ensure patient safety.
Consultants are highly experienced workers, with decades of clinical practice behind them. They receive a secure basic salary that increases as fixed thresholds are reached. An NHS consultant working full-time has a starting salary of £84,559 (Threshold 1). This basic salary is increased yearly, starting at £87,207 at Threshold 2 (1 year of consultant level practice). Thresholds 2 to 5 are achieved per year of practice. Threshold 6 is attained at 9 years, Threshold 7 at 14, and Threshold 8 at 19 years at consultant level (with a basic salary of £114,003). Basic salary is reduced if the consultant works part-time.
Consultants’ incomes vary greatly, depending on how many years of experience they have, how much they work evenings and weekends, how much they are involved in teaching or research, and whether they have a “clinical impact award” – a bonus once called a “merit award”. Some consultants in the UK also supplement their NHS income with private practice, and a few can double their earnings.
For the reasons given above, it is difficult to say with accuracy what the average income of a consultant is. Position in the income distribution may give a clearer idea. In 2022 the top 10 % of UK workers earned around £62,583 a year. This means that a trained NHS specialist enters the top 10% of the income distribution when appointed to a full-time consultant post.
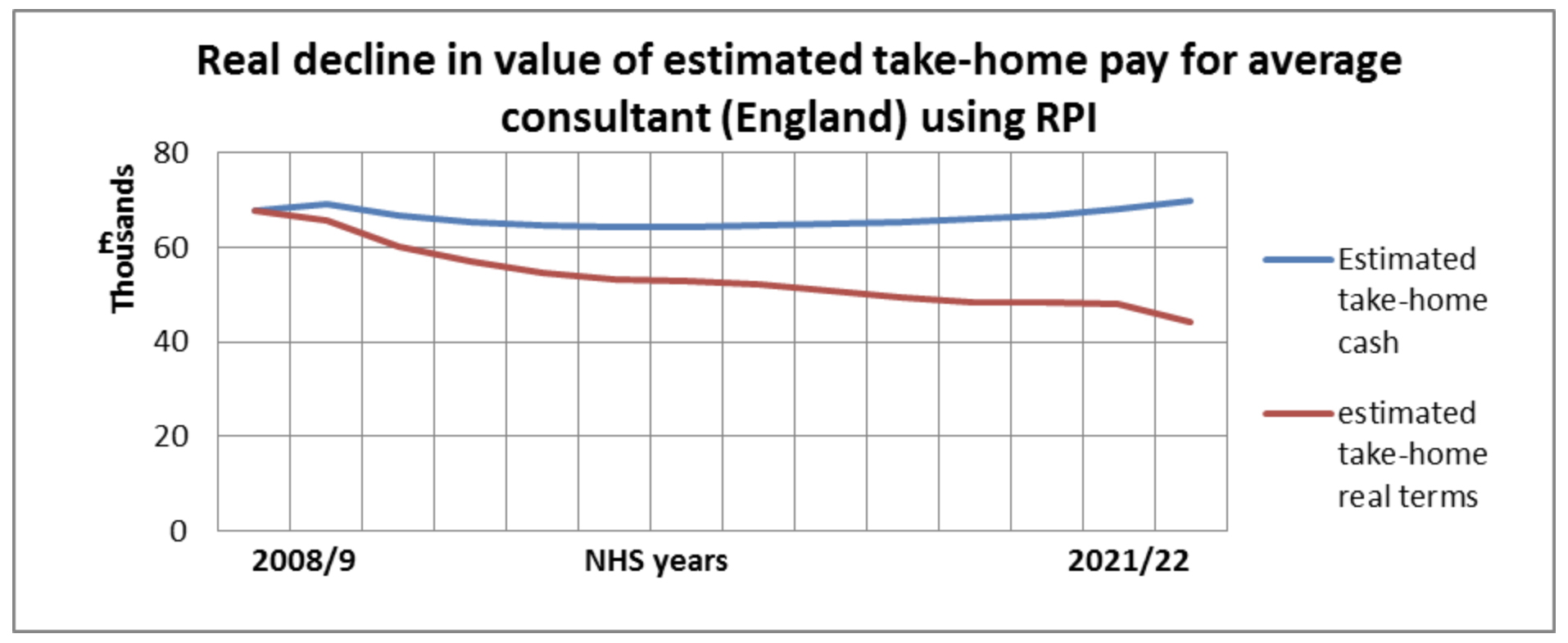
The British Medical Association makes three claims in defence of the strike decision. First, take-home pay has fallen by 35% since 2008/9, and the BMA wants this pay erosion to be reversed. Second, the independence of the Doctors’ Pay Review body (which advises on pay) has been undermined by government and must be restored. Third, working conditions in the NHS are deteriorating and putting patients at risk.
Pay Erosion
The BMA is right about pay erosion, as the graph shows. The top line shows take-home pay between 2008/9 and 2021/22, and the lower line shows take home pay adjusted for purchasing power. The BMA is aware that its consultant members have high incomes and are not as hurt by pay erosion as the junior doctors are. Nevertheless the BMA pursues higher incomes for its consultant members because going the extra mile for those in need of medical care is unsustainable without reward. The BMA’s members are both ‘Knights’ selflessly helping others but also ‘Knaves’ seeking personal gain.
Pay Review
The government seems to have conceded a point here. The Department of Health & Social Care argues that it is taking advice from the Review Body and that consultants have already received a salary uplift of 4.5%. A major concern among consultants is the size of their pension pot over a likely retirement period of 20 to 30 years. Limits on how much can be saved tax-free in the NHS pension have been abolished and the maximum annual allowance (the amount that can be added to the pot each year) has been increased from £40,000 to £60,000.
Working Conditions
The state of the NHS is probably the strongest case in the BMA argument. It is true that the NHS has struggled through the Covid crisis, staff are weary and the backlog of work is growing, but there are deeper problems. Hospital medicine has changed a lot in the last two decades. The change from a team-based approach to work (“The Firm”) to a shift-based system has reduced the number of junior doctors on site at any given time. This intensifies both their workload and that of the consultants, erodes the quality of care and puts the public at risk. One medical ethics commentator argues that “If the conditions that doctors work under put patients at risk, then (on balance) they are morally obliged to strike”. This is Knightly talk, laced with anger at what successive Tory governments have done to the NHS.
What next?
Some consultants are worried by their union’s militancy. They think that industrial action will put patients in harm’s way, endanger them by compromising their safety, create hardship for thousands on waiting lists (if only in the short term) and erode public trust in the medical profession. Not all NHS consultants support strike action with one critic suggesting that medical staff are “… the most protected workforce there is at the moment …. with the best Terms and Conditions and pensions…..I think the public is on the verge of seeing NHS staff as over entitled”. .
Public opinion may start to turn against the BMA’s consultants if they are not seen primarily as noble Knights who protect NHS patients. For example, there is an argument about whether consultants providing medical ‘cover’ for striking junior doctors should be paid a special rate recommended by the BMA or the lower rates paid for normal overtime. This worries some NHS Trust bosses who think that paying higher cover payments during the strike would set a precedent for continued higher routine overtime rates once the strikes end. Compared with the big issues being fought out in this dispute, this is trivial and pure knavishness. How much it troubles the public remains to be seen.
Read more News from Nowhere and articles on the NHS in ERA 3 at http://www.healthmatters.org.uk/
